The Science of Surf Therapy: New Research on Chronic Pain Relief
By Tracey Chester, LMFT, MS, MA
For millions living with chronic pain, healing can feel like an endless cycle of appointments, medications, and explanations that never seem to be enough. Yet, sometimes healing begins not in a hospital room or therapy office — but in saltwater.
At the Pain Trauma Institute, we set out to explore a simple but radical question:
What if the ocean could help heal pain that medicine couldn’t?
From Clinical Care to the Coastline
This study — a collaboration between the Pain Trauma Institute, USC’s Department of Biokinesiology and Physical Therapy, and Groundswell Community Project — invited nine participants living with chronic pelvic pain and other overlapping chronic pain conditions to the shores of Southern California for a series of guided surf therapy sessions.
The group included both women and men, ages 30–62, all of whom had experienced long journeys through the medical system. Many carried not just physical pain, but the invisible weight of medical trauma and dismissal.
Each participant attended four sessions led by certified surf therapists trained in the Groundswell Surf Therapy for Trauma Recovery model. Before and after each surf, we measured changes in pain intensity and emotional state using the McGill Pain Questionnaire (MPQ), self-reported assessments, and real-time EEG brainwave data collected through a 4-channel Muse device.
Our goal was to understand not just how people felt better — but how their brains responded to the ocean itself.
The Results: Measurable Shifts in Pain and Presence
The findings were striking.
Across all participants, we observed an average 50% reduction in pain scores after each surf therapy session.
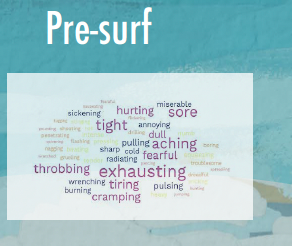
Using the McGill Pain Questionnaire, participants selected 56% fewer pain descriptors after surfing — meaning they described their pain as less intense, less consuming, and less emotionally charged.
One participant summed it up simply:
“On land, my body feels like a problem I have to manage. In the water, it finally makes sense.”
The EEG data told a parallel story.
Those who reported the greatest pain relief also showed the largest increases in delta brainwave activity (2–4 Hz) — a frequency band associated with deep rest, parasympathetic regulation, and nervous system healing. In other words, the brain appeared to mirror the body’s surrender to the sea.
Participants also reported feeling more interested, excited, strong, enthusiastic, proud, alert, inspired, determined, and active after each session. The ocean didn’t just ease pain — it reawakened vitality.
Beyond the Data: Restoring the Right to Belong in Your Body
Behind every number was a story of resilience.
Stephanie, 45, lives with Lyme disease and chronic fatigue:
“On land, my body feels like a problem I have to manage. In the water, it finally makes sense.”
Cat, 29, lives with POTS and connective tissue pain:
“Surfing taught me to meet my body with curiosity instead of judgment. The ocean doesn’t ask for perfection — only presence.”
And Nancy, a 41-year-old nurse with long COVID, shared:
“In medicine, I used to be the helper. After getting sick, I felt invisible. Surf therapy reminded me that I still belong to something alive.”
These voices point to something medicine often overlooks: the emotional and social dimensions of healing. Surf therapy bridges what the medical system tends to separate — the biological, psychological, and communal aspects of health.
As one participant said during our final circle:
“I stopped apologizing for existing in pain.”
The Nervous System in Motion
Blue Mind Science — the study of how water impacts the brain — suggests that proximity to water supports emotional regulation and parasympathetic activation. In surf therapy, this becomes an embodied practice.
Each paddle stroke and wipeout becomes a small act of exposure and recovery. Each wave a reminder that safety can exist even in motion.
Surf therapy gives participants something pain had taken: agency, awe, and belonging.
What This Means for the Future of Pain Care
These findings offer early but powerful evidence that surf therapy can meaningfully reduce pain and support nervous system healing — even among patients with complex, overlapping chronic conditions. More importantly, it restores something harder to quantify: hope.
Our next phase of research aims to expand this work to a larger sample and further explore how surf therapy can complement traditional pain management and trauma recovery approaches.
Because for many, the ocean is more than a backdrop — it’s a co-therapist.
It doesn’t fix you, but it reminds you that you were never broken.
Further Reading
For those navigating the invisible wounds of medical trauma and chronic pain, Tracey shares her personal and professional insights in her book.
In this powerful guide, Tracey shines a light on the silent epidemic of medical trauma — giving voice to those whose pain has too often been dismissed.
Drawing from lived experience and decades of clinical work, she offers:
Tools for navigating the emotional aftermath of medical trauma
Strategies for self-advocacy in a broken healthcare system
A trauma-informed roadmap for healing both body and mind
Reflections on grief, identity, and reclaiming your story
Practices rooted in narrative therapy, somatics, and surf therapy
More than a book, it’s a companion for the journey — a reminder that you are not crazy, alone, or beyond healing.
With Somatic Took Kit by Natalie Small
Written by:
Tracey Chester, LMFT, MS, MA
Founder, Pain Trauma Institute
Partner, Groundswell Community Project
@SDPainTraumaInstitute